
TPN Administered
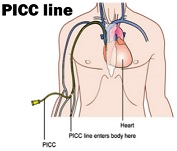
TPN administration into a vein, generally through a PICC (peripherally inserted central catheter) line, but can also be administered through a central line or port-a-cath. Patients may be on TPN for many weeks or months until their issues resolve
Demonstration Videos
Guidelines, Specifications & User Manuals
Helpful Information
Total Parenteral Nutrition (TPN), also known as intravenous or IV nutrition feeding, is a method of getting nutrition into the body through the veins. In other words, it provides nutrients for patients who do not have a functioning GI tract or who have disorders requiring complete bowel rest. At Care+Wear, we have gathered information on the nutritional content of TPN, possible complications of TPN and proper ways to administer TPN.
So, what exactly is TPN? TPN is short for Total Parenteral Nutrition and it provides patients with all or most calories and nutrients through solutions that contain a mixture of protein, carbohydrates, glucose, fat vitamins and minerals using vascular access devices like PICC lines. Other vascular access devices include Peripheral Intravenous line, Midline or Central lines with the central line being the most common access for TPN administration. Examples of common central lines include PICC lines, Hickman catheters, and Groshong catheters. TPN can be administered in the hospital or at home and is most often used for patients with Crohn’s disease, cancer, short bowel syndrome or ischemic bowel disease. However, critically ill patients who cannot receive nutrition orally for more than four days are also candidates for TPN. Other indications that TPN should be used include patients with severe pancreatitis, paralytic ileus, intractable vomiting, diarrhea and high-output fistula (OncologyNurseAdvisor.com).
Typically, TPN requires a solution of water (30 to 40mL), energy (30 to 45kcal), amino acids, essential fatty acids (1 to 2kg), vitamins and minerals. However, TPN solutions will be customized to meet each patient’s individual needs that are based on the patient’s age and organ function status. For instance, patients with heart or kidney disorders may require a limited volume of liquid intake while those with respiratory failure require a liquid emulsion that provides most of the nonprotein calories. The basic adult daily requirements for total parenteral nutrition information can be found through this link.
TPN is also highly common among children and teenagers. Children who are on TPN may have short bowel syndrome, which results from the malfunctioning of the small intestine and other intestinal diseases like microvillus inclusion disease. In fact, according to the Children’s Hospital of Pittsburgh, many children who are on the waiting list for an intestinal transplant are on TPN. TPN is not only used for young children, but is also commonly used for teenagers. However, being on TPN may be most difficult mentally for teenagers since they are highly concerned about their body image. This may result in them disconnecting their TPN before they should or to not use TPN at all. Hence, it may be especially helpful for teens to get in contact with other teens who are also on TPN by joining support groups. For instance, teenagers and their caregivers can join The Oley Foundation, a national, non-profit organization that provides information, services, and emotional support for people on TPN, their families and caregivers.
THEN WHAT ARE THE WAYS TO PROPERLY ADMINISTER TPN?
First, TPN is administered through a needle or catheter that is placed in a large vein that goes directly to the heart called a central venous catheter. Since the central venous catheter needs to remain in place to prevent further complications, TPN must be administered in a clean and sterile environment. For instance, external tubing should be changed everyday and dressings should be kept sterile with replacement every two days.
TPN is usually used for 10 to 12 hours a day, five to seven times a week. Most TPN patients administer the TPN infusion on a pump during the night for 12-14 hours so that they are free of administering pumps during the day. TPN can also be used in both the hospital or at home.
In fact, according to Children’s Hospital of Pittsburgh, approximately 40,000 people in the United States receive TPN at home. However, if TPN is given at home, it is crucial for patients to be given a qualified home nurse in order to better recognize various symptoms of an infection and be taught the correct steps of administering the nutrition. For example, patients must store their prescribed liquid in a refrigerator and remove each dose from the fridge about five minutes before use.
It is also important that the progress be followed and monitored by an interdisciplinary nutrition team. For instance, patients’ weight, CBC and electrolytes level should be monitored daily. In particular, plasma glucose should be monitored every 6 hours until patients and glucose levels become stable. Also, other measurements including liver function tests and full nutritional assessments including BMI calculation and Anthropometric measurements should be repeated at 2 weeks intervals.
WHAT ARE SOME BENEFITS AND RISKS OF TPN?
TPN is beneficial because it provides nutrients that are vital in maintaining high energy, hydration and strength levels. Also, it will allow patients to heal more quickly and feel more energized. It is especially beneficial for children and teenagers because if these two groups do not get all of the nutrients they need, then they may have developmental or growth delays.
However, there are also many risks associated with receiving TPN. The most common risk includes catheter infection with the most serious form resulting in sepsis. Others include blood cots resulting from the line moving out of place. Also, long-term use of TPN may lead to liver disease and bone disease. Hence, it is crucial for patients receiving TPN to be closely monitored for complications by their health care team.
According to the Merck Manual about 5 to 10 percent of patients have complications related to their central venous access device. There are 3 main types of complications: Catheter- related sepsis, Glucose abnormalities and liver dysfunction.
First, glucose abnormalities such as hyperglycemia or hypoglycemia are one of complications resulting from TPN usage. Although treatment for these side effects may depend on the degree of abnormalities, constant monitoring of glucose levels and adjusting the insulin dose in the TPN may be helpful. Moreover, short term hypoglycemia may be reversed with 50% dextrose IV while more prolonged form of hypoglycemia may require infusion of 10% dextrose.
Other types of complications include liver dysfunction, painful hepatomegaly, and hyper-ammonia. First, liver dysfunction may be the result of increased bilirubin and alkaline phosphatases from excess amino acids. As a result, cholestasis and inflammation and progressive fibrosis may occur. Reducing protein delivery may help treat this effect. Painful hepatomegaly and hyper-ammonia are other types of hepatic complications resulting in fat accumulation and feeling of lethargy, twitching and seizures. Other complications include metabolic bone disease, adverse reactions to lipid emulsions, gallbladder complications and abnormalities of serum electrolytes and minerals that can be corrected by modifying subsequent infusions with adequate vitamin and mineral solutions.
In conclusion, receiving TPN can be a life saving method to receiving the required nutrition but like all treatments it requires diligent