What is a PEG tube?
It is a soft, plastic feeding tube that goes into your stomach. Liquid, such as formula, fluids, and medicines, can be put through the PEG tube if you cannot eat or drink all the nutrients you need. It can also be used to take air and fluid out of your stomach.
Demonstration Videos
SPECIFICATIONS
How do I use a PEG tube for feedings?
Your healthcare provider will tell you when and how often to use your PEG tube for feedings. A bolus feeding means nutrition is given over a short period of time. An intermittent feeding is scheduled for certain times throughout the day. Continuous feedings run all the time. The following are types of PEG tube systems:
- A feeding syringe helps liquid food to flow steadily into the PEG tube. The syringe is connected to the end of the PEG tube. You will pour the liquid into the syringe and hold it up high. The syringe plunger may be used to gently push the last of the liquid through the PEG tube.
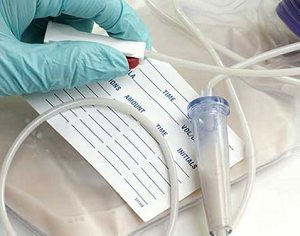
- A gravity drip bag allows liquid food to drip more slowly into the PEG tube. The tubing from the gravity drip bag is connected to the end of the PEG tube. You will pour the liquid into the bag. The bag hangs on a medical pole or similar device. You can adjust the flow rate on the tubing according to your healthcare provider’s instructions.
- An electric feeding pump controls the flow of the liquid food into your PEG tube. Your healthcare provider will teach you how to set up and use the pump.
How do I care for my PEG tube?
- Always wash your hands before and after each use. This helps prevent infections. Use soap and water to wash your hands.

- Always flush your PEG tube before and after each use. This helps prevent blockage from formula or medicine. Use at least 30 milliliters (mL) of water to flush the tube. Follow directions for flushing your PEG tube.
- If your PEG tube becomes clogged, try to unclog it as soon as you can. Flush your PEG tube with a 60 mL syringe filled with warm water. Never use a wire to unclog the tube. A wire can poke a hole in the tube. Your healthcare provider may have you use a medicine or a plastic brush to help unclog your tube.
- Check the PEG tube daily:
- Check the length of the tube from the end to where it goes into your body. If it gets longer, it may be at risk for coming out. If it gets shorter, let your healthcare provider know right away.
- Check the bumper. The bumper is a piece that goes around the tube, next to your skin. It should be snug against your skin. Tell your healthcare provider if the bumper seems too tight or too loose.
- Use an alcohol pad to clean the end of your PEG tube. Clean before you connect tubing or a syringe to your PEG tube and after you remove it. Do not let the end of the PEG tube touch anything.
How do I care for the skin around my PEG tube?
- Do not remove the stitches or medical tape. Stitches or medical tape hold your PEG tube in place when you first get it. Your healthcare provider will take them off once the skin around your tube heals. Leave clean bandages over the tube area for the first 24 hours after the tube is put in. You may not need to use bandages after 24 hours if the skin around the tube looks dry. Ask when you can shower or bathe.
- Routine skin care:
- Clean the skin around your tube 1 to 2 times each day. Ask your healthcare provider what you should use to clean your skin. Check for redness, swelling, or pus in the area where the tube goes into your body. Check for fluid draining from your stoma (the hole where the tube was put in).
- Gently turn your tube daily after your stitches come out. This may decrease pressure on your skin under the bumper. It may also help prevent an infection.
- Keep the skin around your PEG tube dry. This will help prevent skin irritation and infection.
- Use topical medicines as directed. You may need to put antibiotic cream on the skin around your tube after you are done cleaning it.
What else do I need to know about a PEG tube?
- Keep a record of liquids you have each day. You may also need to keep a record of how much you urinate and how many times you have a bowel movement each day. Bring this record to your follow-up visits.
- Check your weight as directed. Keep a record of your weights and bring it to your follow-up visits. Your healthcare provider may need to change your feedings if your weight changes too quickly.
- Take your medicines as directed. Learn which of your medicines can be crushed, mixed with water, and given through the PEG tube. Certain medicines should not be crushed or may clog the PEG tube.
- Go to all follow-up appointments. You may need to have blood tests and other tests when you see your healthcare provider.
When should I call my doctor?
- You start coughing or vomiting during or after a feeding.
- You have severe abdominal pain.
- Blood or tube feeding fluid leaks from the PEG tube site.
- Your PEG tube is shorter than it was when it was put in.
- Your PEG tube comes out.
- Your mouth feels dry, your heart feels like it is beating too fast, or you feel weak.
- You have nausea, diarrhea, or abdominal bloating or discomfort.
- You have stomach pain after each feeding or when you move around.
- You have discomfort or pain around your PEG tube site.
- The skin around your PEG tube is red, swollen, or draining pus.
- You weigh less than your healthcare provider says you should.
- Your PEG tube is longer than it was when it was put in.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
© Copyright IBM Corporation 2019 Information is for End User’s use only and may not be sold, redistributed or otherwise used for commercial purposes. All illustrations and images included in CareNotes® are the copyrighted property of A.D.A.M., Inc. or IBM Watson Health
USER MANUAL
FREQUENTLY ASKED QUESTIONS
Helpful Hints
Percutaneous Endoscopic Gastrostomy (PEG) tube
What is a PEG tube?
It is a soft, plastic feeding tube that goes into your stomach. Liquid, such as formula, fluids, and medicines, can be put through the PEG tube if you cannot eat or drink all the nutrients you need. It can also be used to take air and fluid out of your stomach.
How do I get a PEG tube?
You go to the Digestive Disease Center to get a PEG tube placed. A tool called an endoscope (scope) is used. It is a small camera with a light on a thin, flexible tube. It goes down into your mouth, through your esophagus (food pipe), and into your stomach. The light helps your doctor find the best place to put the PEG tube.
Your doctor will make a small incision (cut in your skin) and put the PEG tube in an opening in your stomach; this is called a stoma. A small balloon is blown up on the end of the PEG tube inside your stomach, and there is a small disc on the outside to hold it in place.
Your health care team will put in an Intravenous catheter (IV) and give you medicine through it to help you relax. This will keep you from having pain while you are getting the PEG tube. Your doctor will also give you local anesthesia. This is a shot of medicine in your skin to numb the area where the cut is made.
What are the risks of getting a PEG tube?
- Damage or bleeding in your esophagus and stomach from the scope
- Infection in your lungs from liquid in your stomach getting into your lungs
- Bruising, pain, and sores around your stoma
- An infected stoma
- The end of the PEG tube moving out of place
- The PEG tube can get blocked, crack, break, and leak
- Your stomach may not empty into your intestines
- An abnormal tissue opening, called a fistula, may form between your skin
- and stomach or intestines.
Will it hurt getting a PEG tube?
You will be given medicines in an IV to help you relax. These will make you sleepy. You may not feel pain or remember the procedure. You may feel pressure or pushing during the procedure.
You can have a little pain after it is put in. You can take mild pain medicine to help with any pain.
How do I get ready for the PEG tube procedure?
Medicines
Your medicines may need to stop or change before your PEG tube is put in. Call the doctor who ordered your medicines at least 2 weeks before your procedure.
- Blood thinners: Call the doctor that orders your medicines such as Coumadin® (warfarin), Plavix® (clopidogrel), Ticlid® (ticlopidine hydrochloride), Agrylin® (anagrelide), Xarelto® (rivaroxaban), Pradaxa® (dabigatran), and Effient® (prasugrel).
- Insulin or diabetes pills: Call the doctor that watches your sugar levels. Your doses may need to change because of the diet needed. Bring them with you on the day of your exam.
Give your care team a list of all your medicines and doses. Tell your care team if you use any herbs, food supplements, or over-the-counter medicine. Tell your care team if you are allergic to any medicines.
One day before your procedure
You may eat and drink as normal.
Do not drink alcohol on the day before or the day of your procedure.
Do not eat or drink after midnight the night before you procedure.
The day of your procedure
We will ask you to sign a legal paper called a consent form. It will tell you about the procedure and the risks. Signing the form gives your doctor permission to place your PEG tube. Make sure all of your questions are answered before you sign the form.
After your procedure
You will stay in a recovery room until you are fully awake and ready to go home or to your hospital room.
It is normal to have a sore throat for two to three days after your exam.
When should I call my doctor?
Call your doctor if:
- The skin around your PEG tube is red, hot, hurts to touch, or has greenish- yellow drainage
- You have a fever
- The tube feels tight around your skin
- The skin around your PEG tube breaks down
- Skin grows over your tube
- Your stoma (the opening in your skin) gets bigger
- You have a lot of leaking around your tube
- Your tube gets blocked
- Your tube is cracked or breaks
- Your tube comes out
- You have nausea (feel like you are going to throw up) or vomiting (throwing up)
- You cannot have a bowel movement
- You have any questions or concerns
How do I take care of a PEG tube?
It may take up to four weeks for the skin around the PEG tube to heal.
Clean the skin around your PEG tube every one to three days or if it is dirty with mild soap and water. Try to gently remove any drainage or crusting on the skin or tube. Then put a new bandage around the tube.
- Do not use any ointments, powders, or sprays around the PEG tube.
- Do not pull your PEG tube. It can move out of place or come out.
- Close your PEG tube and tape it to your stomach when you are not using it.
Can I take a bath or go swimming?
Yes, you can do normal activities after the skin around your PEG tube heals. Be sure it is closed before getting into a pool or tub.
What can I put in a PEG tube?
Liquid, such as formula, fluids, and medicines, can be put through the PEG tube. Do not put pills into your PEG tube.
A dietitian will talk with you about the commercial formulas that are best for you to get a balanced diet with all the vitamins and minerals you need. They will talk to you about how much and how often to give yourself the formula. Use these formulas so your tube does not get blocked.
Before you give yourself medicine or start a feeding, check for:
- Leftover liquid in your PEG tube and stomach
- Cracks or breaks in the PEG tube
Will I give myself feedings at normal meal times?
You can give yourself feedings at any time during the day or night. Some people feed themselves at normal meal times. Some people choose other times during the day or overnight.
No matter when you decide to feed yourself, it still may be nice to sit with your family during meal times to share and talk. Also, be sure you choose feeding times that let you get enough sleep.
How do I give myself medicine through a PEG tube?
You can give yourself medicine that is liquid or finely crushed and dissolved in water. Never mix medicines. Always flush the tube with a little water between each medicine and after the last medicine is given.
Will I taste anything?
Your taste buds are on your tongue, so you will not taste food that is given through your PEG tube. You might be able to taste something if you burp after a feeding.
Can I eat or drink after a PEG tube is put in?
It depends why you needed the PEG tube. Talk to your care team about eating and drinking.
It is normally okay to eat and drink if you needed the PEG tube because of:
- Weight loss
- Not being able to gain weight
- Just in case you are not able to eat enough
If your care team tells you it is okay to eat and drink, you cannot do so until your gag reflex returns.
Talk to your care team about what is safe to eat and drink if you have problems swallowing or if you aspirate (food or drink goes down your windpipe into your lungs), or if you needed the PEG tube to keep your stomach empty. Some people should not eat or drink anything. Some people can eat and drink different amounts and consistencies in certain positions.
What if the PEG tube falls out?
Do not panic if your PEG tube ever falls out. Put a clean, dry towel over the opening to catch drainage and go to your doctor or emergency room to get another tube put in. The opening can close quickly, so get it put back in as soon as you can.
Will the PEG tube leak?
It can leak a small amount. Clean and dry the skin around the tube if it does leak so you do not get skin breakdown or sores.
Keep gauze or absorbent pads on the PEG tube to keep the skin dry and protect your clothes. You may want to take extra pads and clothes with you when you leave your home.
The tube may need to be changed if it leaks more than a little.
Will people know I have PEG tube?
A PEG tube is small and is hidden by your clothing. People will only know you have a PEG tube if you show them.
Will I have a PEG tube forever?
This depends on your weight, health, eating habits, and if you can swallow. You should talk with your care team about this.
RELATED ITEMS
PEG Tube – Enteral Feeding Instructions
What is a PEG tube? It is Read more...
Gastrostomy Tube Instructions
Gastrostomy Tube Enteral Feeding Enteral Nutrition (EN), Read more...
Kangaroo Joey Pump Setup – Enteral Feeding
Kangaroo ePump Enteral Feeding Pump The latest Read more...
Kangaroo Joey Enteral Feeding Pump Instructions
Kangaroo™ Joey Enteral Feeding Pump The Covidien Read more...
How to Unclog Your Enteral Feeding Tube Instructions
How to unclog enteral feeding tube Prevent Read more...
Flocare Infinity Enteral Feeding Pump Instructions
Nutricia Flocare® Pumps Flocare® Infinity™ pumps are Read more...
Compat Ella® Enteral Pump Instructions
COMPAT ELLA® Enteral Feeding pump An innovative Read more...
EnteraLite® Infinity Enteral Pump Instructions
Entera LiteInfinity® Feeding pump A nutrition delivery Read more...